
Speak to a program educator to answer any questions about treatment and support
Connect with a reimbursement navigator to see if you have private coverage
For adults:
Saxenda® (liraglutide injection) is used for chronic weight management in addition to reduced calorie diet and increased physical activity in adults aged 18 and above who have either:
* BMI (Body Mass Index) is a simple measure of your weight in relation to your height. See your doctor to have your BMI measured.
For adolescents:
Saxenda® is also used in addition to a reduced calorie diet and increased physical activity for chronic weight management in adolescents aged 12 to less than 18 years with obesity, as diagnosed by a doctor, who have been unsuccessful on a reduced calorie diet and increased physical activity alone.
Consult your doctor regarding use of Saxenda® in adolescents aged 12 to less than 18 years. Saxenda® is not recommended for use in children under 12 years of age or in adolescents with a body weight below or equal to 60 kg.
Saxenda® helps adults with obesity or overweight, or adolescents with obesity, who also have weight-related medical problems lose weight and keep the weight off. Saxenda® should be used with a reduced calorie diet and increased physical activity.
Yes, it is. Saxenda® is just one part of your weight management plan. Your healthcare team will recommend a reduced calorie diet and strategies to increase your physical activity.
There is no specific recommended diet to go along with Saxenda®. However, Saxenda® should be taken with a reduced calorie diet and increased physical activity.
Speak to your healthcare professional about a reduced calorie diet that is right for you and that you will be able to sustain in the long term.
Below is a dosing schedule to guide you from the starting dosage of 0.6 mg to the full dosage of 3.0 mg.
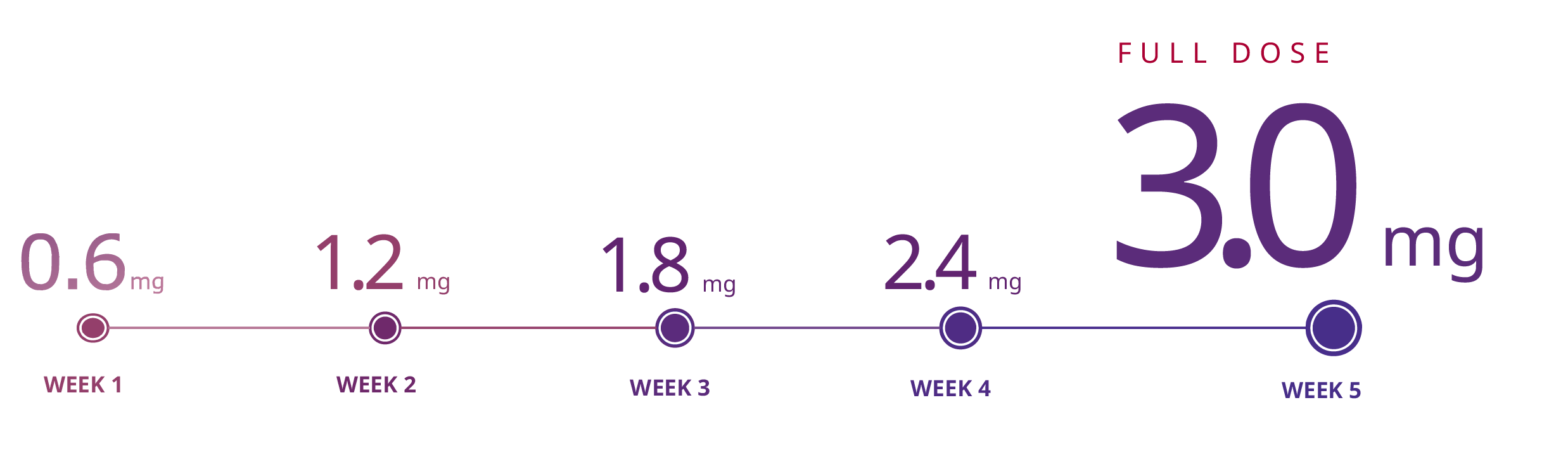
When you first start using Saxenda®, the starting dose is 0.6 mg once a day. Your dose should be increased by 0.6 mg once per week until you reach the 3.0 mg dose. After you reach the 3.0 mg dose, do not change your dose unless your healthcare professional tells you to.
Use Saxenda® exactly as prescribed by your healthcare professional.
You should inject Saxenda® once a day, at any time, with or without food.
To help you remember to take Saxenda®, choose a time of day that works best for you. For example, you can take Saxenda® every morning when you wake up, or when you brush your teeth before going to bed.
Speak to your doctor about a diet and physical activity program when you start taking Saxenda®. Stay on this program while you are taking Saxenda®.
If you miss your daily dose of Saxenda®, take it as soon as you remember. Then, take your next daily dose as usual on the following day. Do not take an extra dose of Saxenda® or increase your dose on the following day to make up for your missed dose.
If you miss your dose of Saxenda® for 3 days or more, call your healthcare professional to talk about how to restart your treatment.
If you think you have taken too much Saxenda®, contact your healthcare professional, hospital emergency department, or regional poison control centre immediately, even if you do not have any symptoms. You may need medical treatment.
Using too much Saxenda® may cause side effects such as feeling sick (nausea), throwing up (vomiting), and/or low blood sugar (hypoglycemia). Low blood sugar may come on suddenly and can include cold sweats, cool pale skin, headaches, a fast heartbeat, feeling sick, feeling very hungry, changes in vision, feeling sleepy, feeling weak, feeling nervous, feeling anxious, feeling confused, difficulty concentrating, and shaking (tremors).
Here is a step-by-step video explaining how to use your Saxenda® pen:
These are some written instructions for how to use your Saxenda® pen. Please refer to the Saxenda® Patient Medication Information for complete dosing instructions.

Check the pen label to make sure it is your Saxenda® pen. Then pull off the pen cap and check that the Saxenda® in your pen is clear and colourless.

Take a new needle and pull off the paper tab. Push the needle straight onto the pen and turn until it is tight. Pull off both needle caps.

Before the first injection with each new pen, check the flow. Turn the dose selector to select the flow check symbol. Hold the pen with the needle pointing up. Press and hold the dose button until the dose counter returns to 0. Make sure a drop appears at the needle tip.
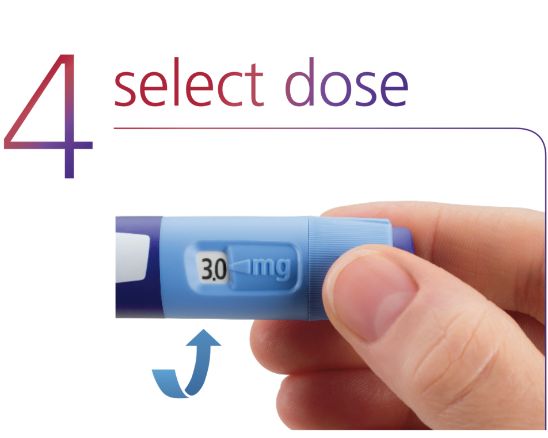
Turn the dose selector to select the dose needed to inject.
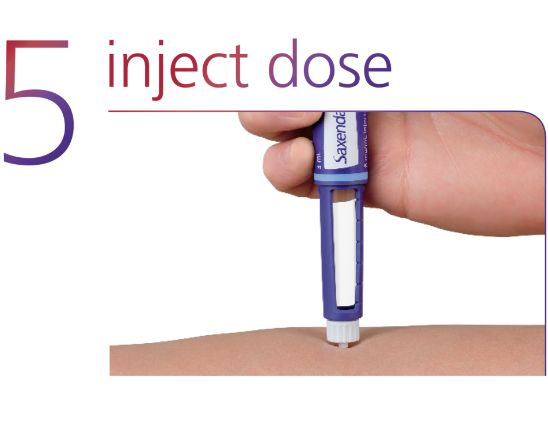
Insert the needle into the skin. Press and hold the dose button until the dose counter returns to 0. Leave the needle in the skin, and count slowly to 6. Then remove the needle from the skin.
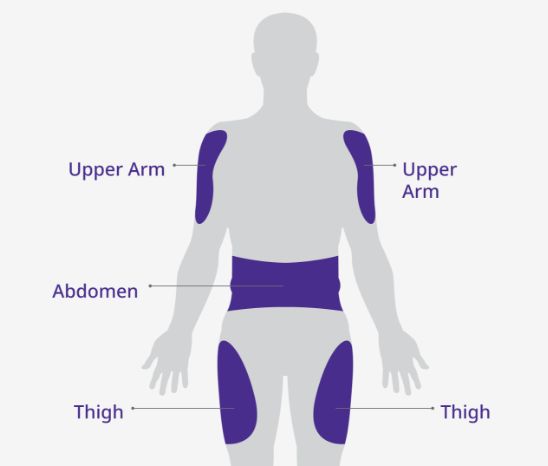
Injection areas
The best places to inject are the front of your abdomen, the front of your thighs, or your upper arms.
Change the place within the area where you inject each day to reduce the risk of developing lumps under the skin.

After the injection, carefully slip the needle into the outer needle cap on a flat surface. Once the needle is covered, unscrew the needle and dispose carefully. Then put the pen cap back on.
In addition, next time you are seeing your healthcare professional, you can show them your injection technique and ask for their feedback.
Having a fear of injections is very common. A strategy to help with your apprehension is to maintain control and determine timing. In other words, take the pressure off yourself to inject. Get the device ready for injection and hold it in your hand. Look carefully at the needle tip, focusing on how small it is. Sit with the device and rest it against the part of your skin where you would inject. Hold it there until you feel calm. You can do this multiple times until you are ready. Most people find that once they give themselves some time to sit with their feelings, they fade (this technique is called desensitization) and rational thinking kicks in—the needle tip is so small, and the sensations associated with injection are equally small.
You can speak to your healthcare professional and ask them to help or give you the first injection.
For questions about treatment and support, do not hesitate to reach out to your live program educator.
Before you start to use Saxenda®, store it in a refrigerator (2˚C to 8˚C) away from the freezer compartment. Do not freeze it or use the pen if it has been frozen.
When Saxenda® is being used, you can keep it for 1 month either at room temperature (not above 30˚C) or in a refrigerator (2˚C to 8˚C).
Do not wash your pen. If necessary, clean it with a mild detergent on a moistened cloth.
Store your Saxenda® pen with the cap on but without a needle attached.
Keep away from sunlight, extreme temperatures, dust, dirt, liquid, and children.
Do not drop your pen or knock it against hard surfaces.
Do not try to fix your pen or pull it apart. If you drop it or think there is a problem, attach a new needle and check that Saxenda® is coming out properly before you inject.
Do not try to refill your pen. Once empty, it must be disposed of.
Do not throw away the pens or needles in the regular trash. Put used needles in a sharps container, which you can obtain at a pharmacy. Ask your healthcare professional about the safe disposal of sharps in your area.
Like all medicines, Saxenda® can cause side effects.
The most common side effects (may affect more than 1 in 10 people) include:
Other common side effects (may affect up to 1 in 10 people) include:
There is a possible risk of thyroid tumours, including cancer, shown with the use of Saxenda® in animal studies. It is not known if Saxenda® will cause thyroid tumours or a type of thyroid cancer called medullary thyroid cancer in people. You should discuss any safety concerns you have about the use of Saxenda® with your doctor.
Tell your doctor if you are taking medication for diabetes as your doctor may adjust your diabetes medication to prevent you from getting low blood sugar. These are not the complete side effects that may occur. For more information, talk to your doctor or read the Patient Medication Information leaflet that comes with your Saxenda® package. Tell your doctor of any side effects not included here or in the leaflet.
If you do experience side effects such as nausea, vomiting, and diarrhea, here are some things that may help:
If you would like more tips to help with side effects, talk to your healthcare team.
Tell your healthcare professional if you are taking, have recently taken, or might take any other medicines. In particular if:
Do not use Saxenda® if:
In addition to monitoring your weight, your physician may ask you to monitor other parameters that they feel are relevant for your individual situation. Speak with your doctor if you have any questions.
Do not stop taking Saxenda® without talking to your healthcare professional.
If you have any questions about Saxenda®, please contact:
Novo Nordisk Canada Inc.
101-2476 Argentia Road
Mississauga, Ontario
L5N 6M1
Regular business hours are:
Monday to Friday from 8:30 a.m.
to 5:00 p.m. EST
Main number: 905-629-4222
Toll-free: 1-800-465-4334
Main fax number: 905-629-8662
Toll-free fax number: 1-844-465-2225
